VR Therapy Impact Calculator
How Much Can VR Help?
Estimate your potential symptom reduction from VR therapy based on your condition and treatment duration.
Virtual reality isn’t just for gaming or fancy demos at tech expos. It’s quietly changing how people heal, learn, and connect-right now, in hospitals, classrooms, and homes around the world. If you’ve ever thought VR was just a flashy gadget, you’re missing the real story.
Healing Minds with Virtual Reality
People with PTSD, anxiety, and phobias are finding relief through VR in ways medicine alone couldn’t offer. A 2024 study from the University of Auckland tracked 120 veterans with combat-related PTSD. Those who underwent 12 sessions of guided VR exposure therapy showed a 68% reduction in symptoms after three months. That’s not a small win-it’s life-changing. The system recreates safe, controlled environments: a quiet street, a crowded bus, even a battlefield. Patients don’t just talk about their fears-they face them, slowly, with a therapist guiding them through every step.
It works for phobias too. Fear of flying? VR simulates takeoffs, turbulence, and landings without ever leaving the clinic. Fear of public speaking? You stand in front of a virtual audience that reacts just like a real one-until you learn to breathe through it. The brain doesn’t know the difference between real and simulated when the sensory input is strong enough.
Rebuilding Bodies After Injury
Physical rehab is boring. Sitting on a stationary bike for 30 minutes, doing the same leg lifts day after day? No wonder people quit. VR turns rehab into a game. Stroke patients in Wellington’s Mercy Hospital now use VR systems that turn arm movements into catching falling fruit or navigating obstacle courses. One patient, a 72-year-old woman recovering from a stroke, improved her arm mobility by 42% in eight weeks-not because she worked harder, but because she forgot she was doing therapy.
For amputees, VR helps with phantom limb pain. By mirroring the movement of their healthy limb on a virtual representation of the missing one, the brain starts to rewire. It’s not magic. It’s neuroplasticity-your brain’s ability to adapt. Companies like Oxford VR have built systems used in over 200 clinics worldwide that combine motion tracking with immersive visuals to make recovery feel less like a chore and more like play.
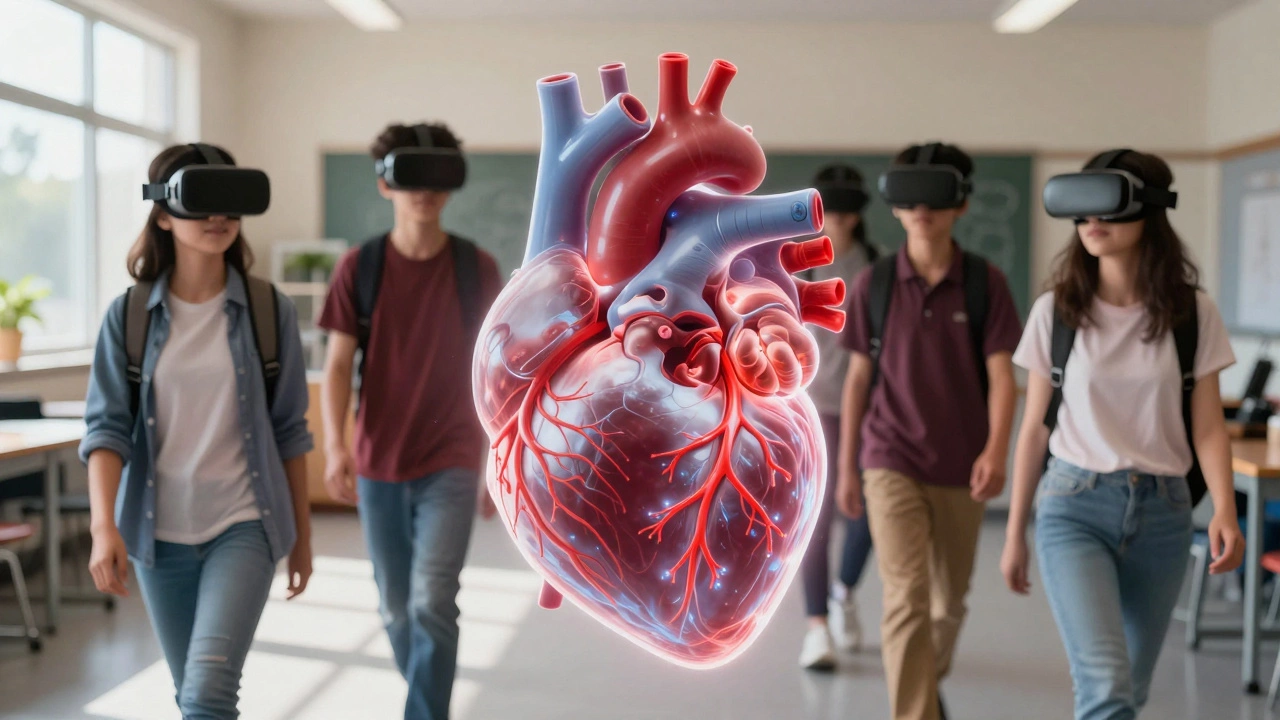
Learning That Sticks
Most students forget 70% of what they learn in class within a week. VR changes that. In high schools across New Zealand, biology classes now use VR to walk through a human heart, watching blood flow in real time. Chemistry students don’t just read about reactions-they mix virtual chemicals, watching explosions and color shifts without a single safety hazard.
Medical students at the University of Otago use VR to practice surgeries before ever touching a real patient. They’ve reduced errors in first-time procedures by 35% since adopting the tech. One trainee told me, “I messed up a virtual liver resection 17 times. When I did it for real, I didn’t even blink.” That’s the power of repetition in a safe space.
Even language learners benefit. Instead of memorizing vocabulary from flashcards, students walk through a virtual Tokyo market, ordering food, haggling over prices, and getting corrected by AI-powered avatars. The immersion makes the brain treat it like real life.

Connecting People Across Distance
Loneliness is a silent epidemic. Older adults, people with mobility issues, and those living in remote areas often go days without meaningful human contact. VR is bridging that gap. Families now gather in virtual living rooms-grandparents watching grandchildren open presents on their birthday, even if they’re on opposite sides of the planet. One widow in Nelson started meeting weekly with a support group in VR after her husband passed. “It felt like we were sitting together,” she said. “I could see their faces, hear their laughter. I didn’t feel alone anymore.”
Workplaces are using it too. Remote teams at tech firms in Auckland now hold meetings in virtual offices. You can point at a whiteboard, pass a virtual document, or even share a coffee together. It’s not perfect-but it’s closer to being in the same room than Zoom ever was.
Therapy for Autism and Developmental Needs
Children with autism often struggle with social cues. A VR program called “Social Skills Coach” lets them practice conversations, reading facial expressions, and handling sensory overload in a controlled environment. One boy, diagnosed with severe social anxiety, went from refusing to speak in class to leading a group project-all after 14 weeks of weekly VR sessions. His teacher said, “He didn’t just learn how to talk. He learned how to connect.”
Adults with developmental delays use VR to practice daily tasks: crossing the street, using public transport, paying at a store. These aren’t abstract lessons-they’re simulations of real-world scenarios that build confidence without the risk of failure.
Why It Works When Other Tech Fails
VR doesn’t just show you something-it puts you inside it. Your body reacts. Your heart races. Your muscles tense. That’s why it’s more effective than watching a video or reading a book. The brain encodes the experience as if it really happened. That’s why VR therapy sticks. That’s why kids remember the circulatory system after walking through a beating heart.
It’s not about the headset. It’s about the experience. A $300 headset can’t fix PTSD by itself. But a trained therapist using that headset to guide someone through their trauma? That’s powerful.
What’s Next?
VR is getting cheaper, faster, and more accessible. By 2027, most public libraries in New Zealand will offer free VR headsets for checkout. Schools are starting to build VR labs instead of just computer labs. Insurance companies are beginning to cover VR therapy for chronic pain and mental health.
It’s not the future. It’s here. And it’s helping real people in real ways-every single day.
Can VR really help with anxiety?
Yes. Clinical trials show VR exposure therapy reduces anxiety symptoms by up to 70% in people with social anxiety, fear of flying, or agoraphobia. It works by letting users face their fears in a safe, repeatable environment, guided by a therapist. The brain learns new responses through repetition, not just talk.
Is VR therapy covered by insurance?
In New Zealand, some private insurers now cover VR therapy for PTSD and chronic pain, especially when prescribed by a licensed clinician. Public health coverage is still limited, but pilot programs in Auckland and Wellington are pushing for inclusion in the national health plan. It’s not widespread yet, but the trend is clear.
Do you need expensive gear to use VR for therapy?
No. While high-end headsets like Meta Quest Pro offer better immersion, many clinics use affordable devices like the Meta Quest 2 or even smartphone-based headsets. The key isn’t the hardware-it’s the software and the trained professional guiding the session. Some apps even work with a simple 360-degree video on a tablet.
Can VR help with physical rehab after surgery?
Absolutely. After knee or shoulder surgery, patients using VR-based rehab programs move more frequently and with better form. Games that turn exercises into challenges-like catching falling objects or balancing on virtual platforms-increase motivation. Studies show patients stick with VR rehab 3 times longer than traditional methods.
Is VR safe for kids?
Yes, when used appropriately. For children under 13, sessions are limited to 20-30 minutes, and content is carefully designed to avoid overstimulation. Schools and therapists use age-appropriate VR for learning and social development. No long-term negative effects have been documented in controlled clinical use.





